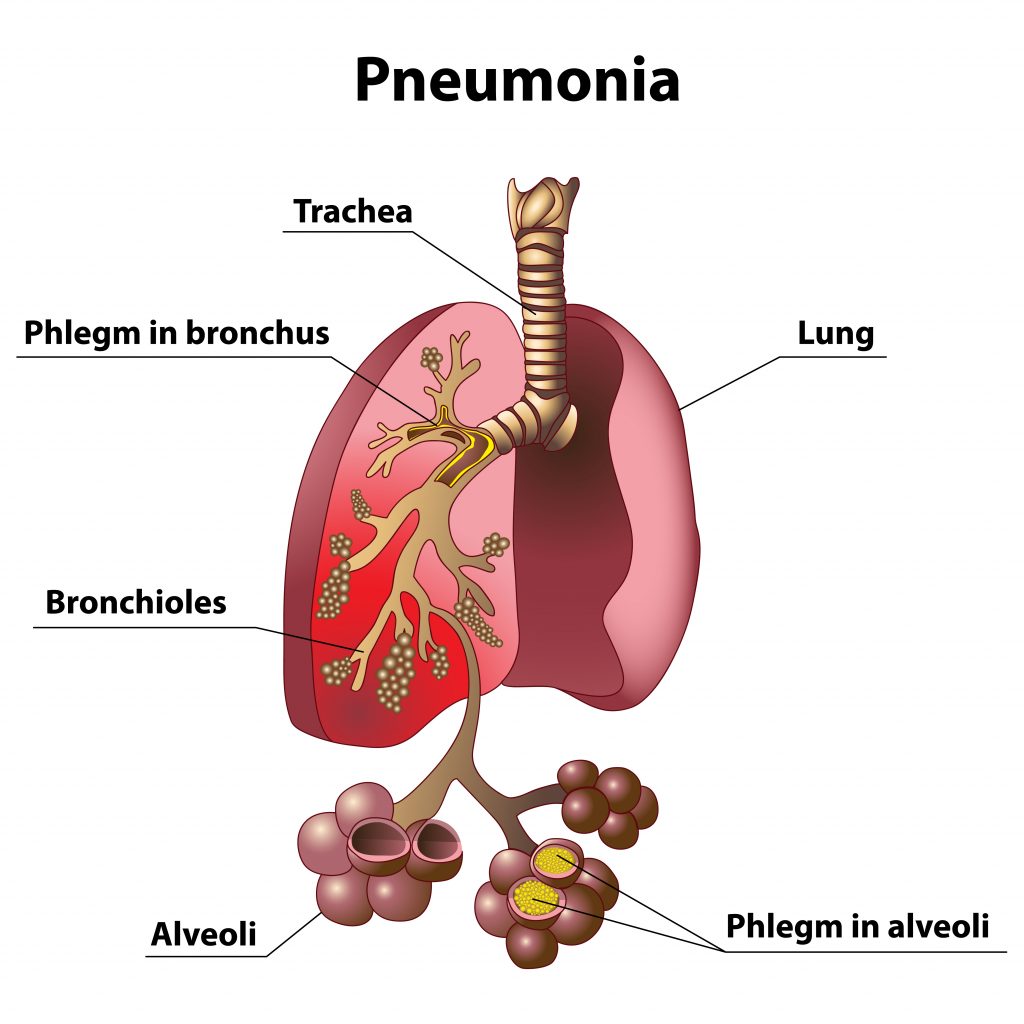
Pneumonia is an infection of the tiny air sacs of the lung called alveoli. Alveoli absorb oxygen from inhaled air. When alveoli become infected, they fill up with fluid, making transport of oxygen throughout the body difficult. Pneumonia can range in severity from a mild illness to a severe, even life-threatening illness.
2.56 million people died from pneumonia in 2017. Almost a third of all victims were children younger than 5 years, it is the leading cause of death for children under 5. (after premature birth)
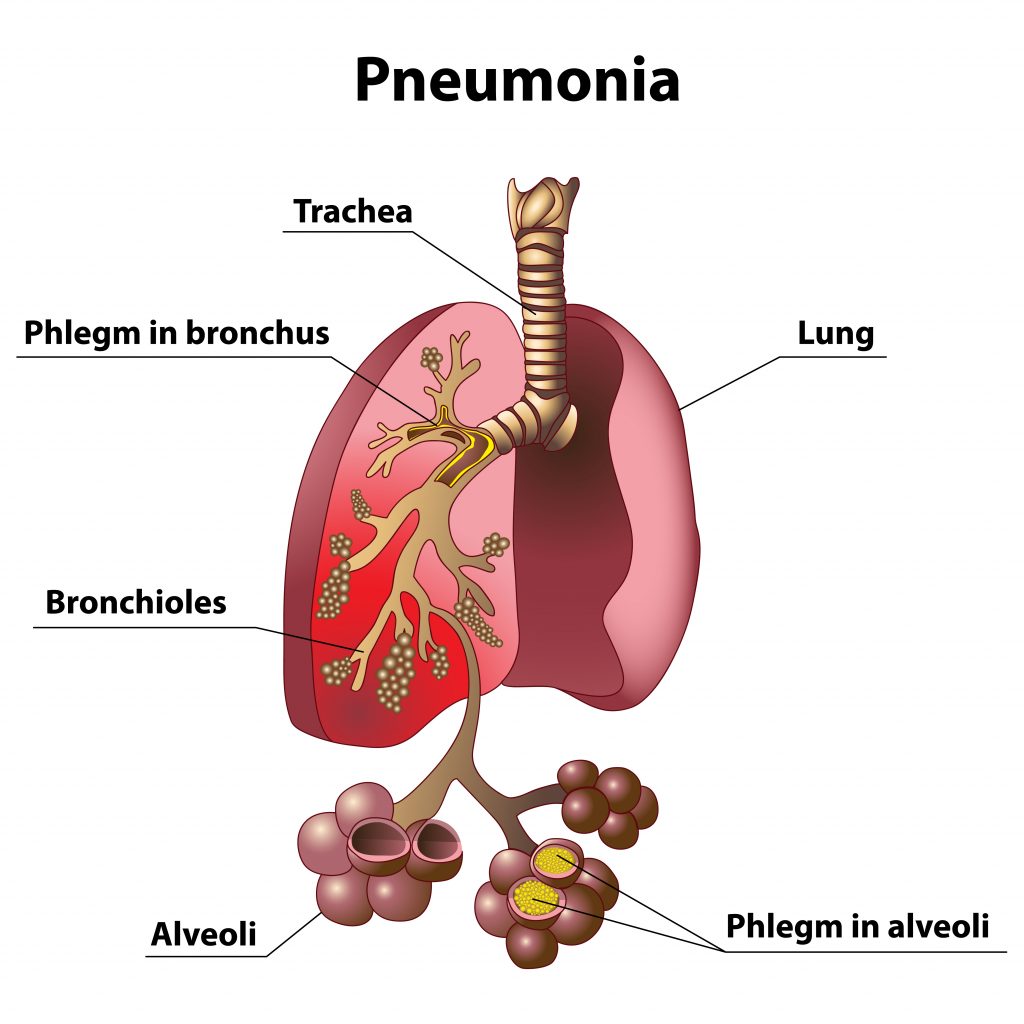
Phlegm in the lungs during pneumonia
Who gets pneumonia?
Pneumonia is a very common illness, which any person can develop. People more likely to get pneumonia include adults 65 years or older, children younger than 5 years old, people who smoke, people with ongoing health conditions, such as chronic obstructive pulmonary disease (COPD), diabetes, congestive heart failure, sickle cell anemia, or conditions that weaken the immune system, such as HIV/AIDS, cancer therapy, or organ transplantation. Pneumonia might also be more likely to occur after some kinds of lung injury – for example, after lungs have been damaged from breathing in chemicals.
How is pneumonia spread?
Some germs that cause pneumonia can spread through the air, by direct contact with an infected person, or by contact with contaminated objects. Some causes of pneumonia can come from the environment and can be spread in dust or other fine particles (e.g., water vapor). Some germs that cause pneumonia are not spread from person to person – for example, a person who loses control of breathing (e.g., during a seizure or while intoxicated) could vomit and then inhale stomach contents and bacteria into the lungs and develop pneumonia.
There are 3 types of pneumonia. Bacterial, viral and fungal pneumonia.
Bacterial pneumonia. Pneumococcal disease is caused by bacteria called Streptococcus pneumoniae and is the most common type of bacterial pneumonia. Other bacterial causes of pneumonia are Haemophilus influenzae, Mycoplasma pneumoniae Staphylococcus aureus (commonly found in healthcare settings), Chlamydia, Legionella species. Bacterial pneumonia is treated with antibiotic therapy. A vaccine is available for some strains of bacterial pneumonia.
Pneumococcus bacteria can cause infections in many parts of the body, including
- Lungs (pneumonia)
- Ears (otitis)
- Sinuses (sinusitis)
- Brain and spinal cord tissue (meningitis)
- Blood (bacteremia)
Complications of pneumococcal pneumonia include:
- Infection of the space between membranes that surround the lungs and chest cavity (empyema)
- Inflammation of the sac surrounding the heart (pericarditis)
- Blockage of the airway that allows air into the lungs (endobronchial obstruction), with collapse within the lungs (atelectasis) and collection of pus (abscess) in the lungs.
- Walking pneumonia- Mycoplasma pneumoniae bacteria commonly cause mild infections of the respiratory system. The most common illness caused by these bacteria, especially in children, is tracheobronchitis (chest cold). Lung infections caused by M. pneumoniae are sometimes referred to as “walking pneumonia” since symptoms are generally mild. Sometimes M. pneumoniae can cause more serious lung infections that require care in a hospital.
Viral pneumonia cannot be treated with antibiotics. Antivirals are sometimes prescribed, along with symptom management. Common causes of viral pneumonia are influenza, respiratory syncytial virus (RSV), and SARS-CoV-2 (the virus that causes COVID-19).
NOTE: Secondary infection of bacterial pneumonia can happen after a person becomes ill with influenza or another virus. At that point, an antibiotic would be indicated.
Fungal pneumonia is caused by the inhalation of spores and is difficult to diagnose. It is estimated that up to 20% of people infected are unaware they have it. It can sit latent for years, and sometimes resolve itself on its own. It is treated with antifungal medication.
The signs and symptoms of pneumonia
- Cough, which may produce greenish, yellow, or even bloody mucus
- Fever, sweating, and shaking chills
- Shortness of breath
- Rapid, shallow breathing
- Sharp or stabbing chest pain that gets worse when you breathe deeply or cough
- Loss of appetite, low energy, and fatigue
- Nausea and vomiting, especially in small children
- Confusion, especially in older people
When to call the doctor
If pneumonia is suspected due to symptoms and the patient is under the age of 5 or immune-compromised or has other risk factors such as heart or lung disease, smokers, asthmatics, and diabetics call healthcare provider. Early detection can lead to reduced hospital stays can be lifesaving.
Call your healthcare provider for the following symptoms if the above risk factors don’t apply:
- Bluish tinge to lips, fingers
- Difficulty in taking deep breaths
- Chest congestion which is painful when breathing
- Consistent fever of 102 or above degrees Fahrenheit
- A hacking cough which produces phlegm or pus
- A fever that resolves then comes back after a few days. This can be an indicator that a viral illness has a secondary bacterial pneumonia in addition to the virus.
How are different types of pneumonia classified?
The various types of pneumonia are classified according to a number of characteristics. To treat these types, it’s essential to know whether somebody caught pneumonia at home, in a hospital, or in a nursing home.
Community-acquired and nosocomial pneumonia
If you develop pneumonia at home, it’s referred to as community-acquired pneumonia (or CAP for short), even if you are admitted to the hospital during the course of the illness.
If you develop pneumonia while in the hospital, it is called hospital-acquired (HAP for short) or nosocomial pneumonia. Pneumonia is considered to be nosocomial if it starts at least two days after you are admitted to the hospital, or within three months of a hospital stay.
Doctors can also classify pneumonia even more exactly, considering whether somebody became infected in a retirement or a nursing home, at a medical facility such as a dialysis center, or while receiving artificial respiration.
Why is classification important for the treatment?
Community-acquired pneumonia is usually caused by pneumococci, whereas nosocomial pneumonia is often connected with staphylococci, various intestinal bacteria, and special germs such as Pseudomonas aeruginosa. Some of those bacteria can be multi-resistant, meaning they are resistant to several antibiotics. That is why different antibiotics are usually needed then for treating community-acquired pneumonia.
Mild, moderate or severe pneumonia
To be able to provide the right treatment, doctors also classify community-acquired pneumonia as mild, moderate, or severe.
Pneumonia is considered to be mild with no increased risk if the patient is:
- is younger than 65 years old,
- is conscious and lucid,
- has normal blood pressure and pulse,
- is not breathing too fast (fewer than 30 breaths per minute),
- has enough oxygen in their blood,
- has not been given any antibiotics in the past three months,
- has not been in the hospital in the past three months, and
- does not have any other severe medical conditions.
People with mild pneumonia can be treated at home and are given antibiotics or antivirals in tablet form.
Symptomatic treatments for mild pneumonia include:
- Over the counter pain reliever reducers such as Tylenol, Advil or Aleve (Note: do not give aspirin to young children)
- Expectorants to help thin out secretions and bring up phlegm
- Avoid smoke and secondhand smoke
- Use a humidifier
- Steamy baths help open airways
- Warm fluids, keep hydrated to thin secretions and bring up phlegm
Avoid cough suppressants unless recommended by your healthcare provider.
The signs of moderate pneumonia include drowsiness and confusion, low blood pressure, worsening shortness of breath, and risk factors such as old age and underlying diseases. People with these symptoms need to have treatment at a hospital. Some will be given a combination of two different antibiotics, at least at the beginning of the treatment.
Pneumonia is classified as severe when the heart, the kidneys or the circulatory system are at risk of failing, or if the lungs can no longer take in enough oxygen. Treatment with an antibiotic infusion in intensive care is then usually needed, sometimes with artificial respiration or additional drugs such as corticosteroids.
Pneumonia in children is only classified as either “not severe” or “severe.”
A word about phlegm/sputum
There seems to be confusion about the color of phlegm/sputum and what it means as far as the infection is concerned. Yellow or green phlegm or sputum can be indicative of an infection. However, viral bronchitis presents as green sputum as a normal feature as does bacterial load from those with COPD. Given the rising incidence of antibiotic resistance sputum or phlegm color should only be one of other symptoms associated with the initiation of antibiotic therapy.
How can pneumonia be prevented?
How long can an infected person carry the germs that cause pneumonia?
Most people who are exposed to the germs that cause pneumonia do not become ill or develop only mild respiratory illness. Fewer develop pneumonia. How long a person can spread a respiratory germ depends on the type of germ and the treatment the person receives (antibiotic therapy, etc.) For some cases of pneumonia, such as influenza or tuberculosis individuals need to stay home until they are no longer contagious. Consult your primary health provider for guidance in these instances.
One of the most important medical preparedness items to store and have readily available is clean water. According to the CDC about 7.2 million people every year in the United States fall ill due to waterborne diseases.
During or shortly after a natural disaster, such as a fire, earthquake, tornado, hurricane, or other inclement weather one of the first parts of the infrastructure that we rely on and fail is our public water supply. If the water supply is disrupted the risk for waterborne disease goes up. If this happens our toilets won’t function properly(if at all), our ability to cook, bathe and drink clean water is compromised. We lose the ability to sufficiently take care of our waste. This can lead to water contamination.
In 2014 in the United States, 17 waterborne pathogens caused an estimated 7.15 million illnesses, 601,000 emergency department visits, 118,000 hospitalizations, and 6,300 deaths. They incurred $3.3 billion in direct healthcare costs, which includes insurance and out-of-pocket payments.
Every year, more people die from unsafe water than from all forms of violence, including war.

In this article we will discuss:
- Common waterborne pathogens that cause illnesses
- How much water to store and how to disinfect water
- Where to find containers to store water
- Choosing a water filter
- This week’s steps to take
Note this is not an exhaustive list, just a sample of waterborne pathogens)
Common waterborne pathogens that cause gastrointestinal symptoms, such as
vomiting and diarrhea
(Please refer to “How to Treat Diarrhea” page)
- campylobacteriosis
- cryptosporidiosis
- giardiasis
- norovirus infection
- Shiga-toxin producing Escherichia coli (STEC) infection O157
- non-O157 STEC infection
- salmonellosis
- shigellosis
- vibriosis (including infections caused by Vibrio alginolyticus, parahaemolyticus, vulnificus and other species)
Waterborne pathogens that cause respiratory symptoms:
- Legionnaires’ disease
- nontuberculous mycobacterial (NTM) infection
- Pseudomonas pneumonia
- Waterborne pathogen that causes skin infection
- Pseudomonas septicemia
How much water to store and how disinfect water

(Taken from CDC website, along with notes and observations in italics)
- Store at least 1 gallon of water per person per day for 3 days for drinking and sanitation
- Try to store a 2-week supply if possible.
- Note: My husband and I live in the mountains, our well was down for a few weeks. 1 gallon of water per person is not enough to sustain life and provide adequate hygiene. I recommend at least 2 gallons, preferably 3 per day for 2 weeks per person)
- Consider storing more water than this for hot climates, pregnant women, and persons who are sick.
- Diarrhea, vomiting, fever and other acute illnesses require increase liquid intake. Storing water after the fact makes no sense. Just be sure to have sufficient water supply on hand before an emergency or grid down situation.
- Observe the expiration date for store-bought water.
- Replace non-store-bought water every 6 months.
- Or sanitize and purify the water before using it.
Store a bottle of unscented liquid household chlorine bleach (label should say it contains between 5% and 9% of sodium hypochlorite) to disinfect your water, if needed. Before filling with safe water, use these steps to clean and sanitize water storage containers:
- Wash the storage container and rinse completely with water.
- Sanitize the container with a solution made by mixing 1 teaspoon of unscented liquid household chlorine bleach in 1 quart of water. Use bleach that contains 5%–9% sodium hypochlorite.
- Cover the container tightly and shake it well. Make sure the sanitizing bleach solution touches all inside surfaces of the container.
- Wait at least 30 seconds and then pour the sanitizing solution out of the container.
- Let the empty sanitized container air-dry before use OR rinse the empty container with safe water (water that has been treated).
- Pour clean water into the sanitized container and cover with a tight lid
Another way to sterilize water (but doesn’t remove chemicals) is solar sterilization. This method utilizes the UV sterilization effect from the sun. It is best done between the 15th and 35th latitude North and South (near the equator) Plastic or glass bottles are set out in the sun for a period of time. Check out the process here:
Where to find containers to store water
When my husband and I started our journey to medical preparedness and self-sufficiency we purchased 5-gallon blue water totes at our local Walmart. These can be found in the camping section of almost any box or sporting goods store. They are fairly inexpensive, store well, are sturdy, and can be moved easily (given the fact that water is very heavy this is a bonus) We now have water stored on our property in 55-gallon food-grade plastic barrels, along with several of these totes.
By the way, a popular item called a water BOB which is essentially a bladder you place inside your bathtub and fill with water. These can be found online. The advantage is that you fill these just before an anticipated event. The disadvantage is if the event is not anticipated you won’t be able to use these.
Other ways to store water
I have sanitized and stored water in glass containers from food (think spaghetti sauce containers) we had consumed. Another way is to use empty, sterilized soda bottles. Used juice bottles with lids work, also. We keep a few gallons of water stored in juice bottles in our car for emergencies, also.
Swimming pools as a source of water
There has been debate over whether drinking swimming pool water in an emergency good practice is. I personally would still filter it for chemicals and organic matter. Or use it to wash clothing and dishes, etc.
Water Catchment system
Water catchment systems are a great way to capture and store water. However, not all states and municipalities allow this. I am a member of the ARCSA ( American Rainwater Catchment Systems Association. They have many free courses and guides on how to safely catch and store rainwater. I highly recommend this organization. They helped us with setting up a catchment system to water our gardens. Many cultures utilize this system for their primary drinking water.
Choosing a water filter
The topic of water filters is a vast one.
When choosing a water filter be sure to choose one that can not only filter out bacteria but also chemical pollutants
I recently purchased the Lifestraw Flex ( I found this link through REI and it is on sale right now) to store with my preparedness supplies. It removes bacteria, protozoa and reduces VOCs and chemicals. It uses no electricity and has its own attached container.
Other water filtration systems that are highly recommended are the Berkey water system. This system is pricey and may be out of the reach for some.
If you do an online search you will come across many ways to filter water from lakes, rivers, ponds, puddles. Charcoal with sand is another way to filter water. Here is a paper describing how to filter water from Utah State University
On a side note- putting together a port a potty and privacy tent is easy and stores in a small footprint. If your toilet isn’t working you will be glad you have this!
You will need the following:
- 5-gallon plastic bucket
- Bags to line bucket
- Baby wipes for cleaning
- Hand gel
- Gloves to remove bags
- Snap on toilet seat found in the camping section of any sporting goods store
- There are products on the market that you can put in the bottom of the plastic bag for absorption and smell. We have used in the past cedar shavings. Baking soda works well, also.
- A pop-up shower tent for privacy
- All the supplies except the tent can be stored in the bucket (just snap the seat on).
Clean water for drinking and hygiene is a necessity. It should be a priority when planning your medical preparedness kit.
This week’s steps to take:
- Take note of how much water you will need for your immediate household.
- Plan for a water supply in your vehicle.
- Decide on where the best place to store the water (preferably a cool, dark area)
- Once you have done this, purchase or clean and repurpose containers to store adequate water. Be sure to label and date the containers.
- Download the article on the management of diarrhea and place in your notebook.
- Bonus step will be to put together the port-a-potty
Our healthcare systems are strained beyond capacity. From healthcare worker shortages to increase in patients visiting the emergency rooms, to medication shortages our fragile healthcare system is reaching, and in some instances has reached crisis mode.
Our medical supplies and medications are in jeopardy
We rely on other countries for the materials to make our medications

According to the council on foreign relations “It is believed that about 80 percent of the basic components used in U.S. drugs, known as active pharmaceutical ingredients (APIs), come from China and India, though the exact dependence remains unknown since no reliable API registry exists.”
(API refers to active pharmaceutical ingredients)
Considering the current healthcare crises, along with the political and social climate of our world, that is a very scary statement.
Our global economy, which virtually shut down over the past months has placed our healthcare system in jeopardy. Even those we rely on during a crisis- our firefighters, EMTs, paramedics are in short supply, or in some areas of the United States they are nonexistent. In many ways we are on our own.
Are you prepared to handle a medical emergency?

According to the CDC there are 130 million visits annually to the emergency room.
Some of the most common reasons for these visits were cough, headache, fever and vomiting.
Many of these visits could be avoided with proper education, supplies and medications on hand.
Medical emergencies come in many forms
- Natural disaster– earthquake, tornado, hurricane, fire, flooding
- Health emergency– heart attack, uncontrolled diabetes, choking
- Illness– fever, vomiting, diarrhea, cough, severe allergic reaction, etc.
- Injury– Motor vehicle crash, household injury such as falls resulting in fracture or sprain,
Etc.
- Supply chain disruption– limited or lack of necessary medications and supplies
What can you do?
First identify your own situation and medical needs
- Are you in an area that is prone to natural disasters?
- Do you live in an area where medical attention may take a long time coming?
- Given the current shortage of EMTs and paramedics you may have a very long wait, even if you live in the city. Be prepared for the fact help may be long in coming or not at all
- Are you or those in your household on medications that would be life threatening if you/they ran out?
- How is yours and household members mobility?
- Do you live alone or with others? If so, would they be able to provide medical assistance if you needed help?
Each household will have a different set of priorities. However, there will still be many common areas to prepare
ACTION PLAN
ACT, NOT REACT
Medical preparedness, just like any preparedness topic has a learning curve. But armed with knowledge, practice, and the necessary medications and supplies you will be able to handle many medical emergencies and avoid a trip to the hospital or clinic.
Get out a notebook and start your action plan if you haven’t already
Start a checklist with the following information:
- Accumulate the necessary food (according to diet -low sodium, diabetic, allergy free foods- and clean water. Goal is to start with a months’ worth of food and build from there. There are several online resources that can help you with this. This may not seem like a medical prep, however without adequate clean water and food you aren’t able to maintain health.
- Discuss with your primary care provider about prescribing several months’ worth of medications AND OBTAIN THOSE MEDICATIONS.
- Schedule a consultation with a Jase medical provider and purchase the antibiotic kit on this site.
- Purchase an adequate first aid kit (It is advisable to have one for each vehicle and a home kit) A recommended website for your first aid kit and other emergency supplies is https://mymedic.com/ Be familiar with what is in the kit, don’t just buy it and put it on the shelf for when emergency arises.
- Along with a first aid kit make sure you have adequate pain relievers, creams, bandages, ace wraps ice packs, etc.
- Post important phone numbers in a place that all in your household know where to find it (911, fire, police, trusted neighbors, family to contact in case of emergency) A self-laminating pouch is a good idea to store this in. The refrigerator or inside a cupboard are common areas these are posted.
- If you and able-bodied members of your household haven’t already attended first aid and CPR classes, sign up and get that done. There are many CPR and first aid course out there. Either find a reputable one locally or the Red Cross has many options to choose from
- Start a first aid library and read the books. Apply what you learn in practice scenarios if able. A few recommended books are American Red Cross First Aid-Responding To Emergencies and The Survival Medicine Handbook- The Essential Guide When Help is NOT on the way
The most important step you can take is to take that first step.
- Get educated
- Obtain supplies
- Practice and get familiar with your supplies.
Next week we will be starting a series on various medical conditions and when to call the doctor.
Our expertise at JASE is focused on providing our patients with the more difficult to obtain prescription medications for their emergency preparedness. Specifically, antibiotics and medications for chronic conditions. Our five specially selected antibiotics can all be found on the WHO’s Model List of Essential Medicines. However, when putting together a useful first-aid/med kit you should include much more than just prescription antibiotics. Here are a few other important medications to consider:
Acetaminophen (Tylenol): Everyone is familiar with this medication. It is a great option for mild to moderate pain. It is safe for those who may have kidney or GI problems as it is processed mainly by the liver and doesn’t cause the same kind of stomach/intestinal issues that ibuprofen can cause.
Ibuprofen (Advil): Another very common and effective medication to treat mild to moderate pain and inflammation. Ibuprofen is processed in the kidneys so caution should be exercised in people who have kidney disease. It can also be hard on the stomach and has been known to cause GI bleeds (although this is rare).
Loperamide (Lomotil): Not all diarrheal causes are from bacteria. Most of the time a diarrheal illness will be self-limited (meaning it will go away on its own without any treatment). Having some loperamide on hand is great when stopping every few minutes to go to the bathroom just isn’t an option. You may be traveling, on a bus or plane, hiking, or at work when you don’t have quick access to a bathroom. Caution when taking this medication as it can sometimes work too well and you will end up with constipation instead! Take as directed and follow the dosage guidelines.
Diphenhydramine (Benadryl): This medication should be in everyone’s first-aid kit. It is an antihistamine and can be used for minor allergic reactions or even as a sleep-aid.
This is just a very small list of over-the-counter medications to consider when putting together a first-aid/med kit. And don’t forget those daily chronic medication needs such as medications for high blood pressure, thyroid disorders, seizure disorders, antidepressants, asthma, etc. Our physicians can determine which medications would be appropriate to prescribe in long-term amounts. Have any questions? Don’t hesitate to reach out to us at answers@jasemedical.com.
A common concern we get from patients is their penicillin allergy. Penicillin reported allergy is the most common drug allergy in the United States. Estimates range from 10%-25% of the population have a penicillin allergy reported on their medical record.
However, even though you might have a penicillin allergy reported on your medical record it doesn’t necessarily mean you have a true allergy. In fact, over 90 percent of patients with a reported penicillin allergy are found to not actually have any allergy when formally tested.
LESS THAN 1 in 10 of reported penicillin allergies are truly allergic
WHY ARE THERE SO MANY FALSE PENICILLIN ALLERGIES?
One of the more common reasons that a penicillin allergy might be posted on a medical record is if a patient took penicillin as a baby and a rash appeared. Rashes are common in sick children and there is a good chance that it was unrelated to the medication. Also, many patients outgrow this kind of sensitivity.
80% of patients who may have once been allergic lose their penicillin sensitivity after 10 years
WHY DOES IT REALLY MATTER? I CAN JUST USE A DIFFERENT KIND OF ANTIBIOTIC.
There are a few reasons why a false penicillin allergy matters. Using the right first-line-directed therapy is in the best interest of the patient. Other medications may be more prone to secondary complications like causing an overgrowth of bacteria in the gut called clostridiodes difficile. C. diff infection causes a difficult to treat diarrheal illness. In addition, other treatments may not be as effective resulting in worse outcomes, longer hospital stays, and higher costs.
HOW DO I KNOW IF MY ALLERGY IS REAL OR NOT?
Your primary care provider can provide a referral to an allergy specialist. The specialist can perform tests including skin testing and even potential treatments like desensitization. If the skin test is negative, then you can safely remove the penicillin allergy from your medical record!
Check out these additional resources:
Is it Really a Penicillin Allergy?
Think You’re Allergic to Penicillin? Why You May Be Mistaken