After antibiotics, Restoring Gut Health
Antibiotics are literally lifesaving. In the most dire of circumstances they can bring someone back from the brink of death. They are powerful medicines. Our lives have greatly benefitted from the use of antibiotics, whether we have used them or not. They have saved millions of lives and the lives of our animals. At Jase medical we take antibiotic stewardship very seriously and advise only using them under the supervision of your healthcare provider. There is much concern over the use of antibiotics and its ability to wipe out the delicate flora of our gastrointestinal system. This concern is founded.
Antibiotics anti- against, biotic- life- against life.
Once someone starts a course of antibiotics the entire course must be completed to kill the invading organism. This comes at a cost to our bodies, however. While the antibiotic kills off the harmful organism it also kills off beneficial bacteria. A study titled “ Short-Term Effect of Antibiotics on Human Gut Microbiota” revealed that after taking certain antibiotics there was up to a tenfold decrease in gut microbiota. Some studies show gut bacteria can return to normal within 6 months. Other studies conclude it can take years. There is much debate over this topic. The type of antibiotic, age, sex, and overall health contribute to gut health and bacterial diversity returning to normal.
This can result in an opportunistic bacteria or yeast to overtake and invade the body. Some people are prone to yeast infections during the course of therapy. Sometimes prescription antifungals are used, in other instances a diet rich in probiotic rich yogurt, over the counter creams and mouthwashes can help.

Our gut houses our immune system
Our immune system is housed in our intestines in tissue known as GALT- gut associated lymphatic tissue. Over 70 percent of our immune system is housed in this tissue, and when taking oral antibiotics, it puts a strain on this part of our immune system. Some of the cells the GALT produces prevent pathogens from adhering and taking up residence in our intestines. The GALT also includes Peyers patches. These patches, which are very similar to spleen cells, line the intestine and house white blood cells. They monitor and kill pathogenic bacteria and viruses when healthy and functioning. They also play an important role in in anti-inflammatory responses. Use of antibiotics puts a strain on this important and not too often talked about system.
In order to restore health to our entire gastrointestinal system functional medicine has come up with the acronym known as the 4 Rs to gut health- remove the offending substance, replace with beneficial foods and bacteria, reinoculate and repair the damage. There is no real definite way to repair the damage, however a diverse gut microbiome helps fight off a variety of pathogenic bacteria.
These steps should be taken during antibiotic therapy and should be a part of a health promoting lifestyle if not already in place.
Remove offending substance
This step can include removing foods that can cause opportunistic bacteria to grow, such as sugar and processed foods, sodas, and high sugar juices. In addition, avoid alcohol, cigarettes, and stress. These suppress the immune system and can make healing the gut very difficult.
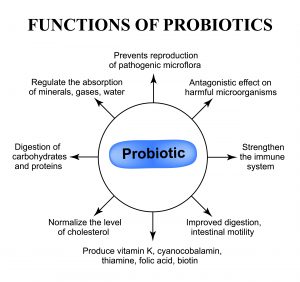
Replace with probiotic and prebiotic rich foods and probiotics
Probiotic rich foods
Probiotic rich foods help inoculate the gut with beneficial bacteria and promote include yogurt with active cultures, kefir, fermented foods such as sauerkraut, kimchi, tempeh, other fermented vegetables and kombucha. You don’t need a lot of these foods to benefit. A tablespoon of sauerkraut provides a group of bacteria called lactic acid bacteria which evidence shows helps fight cancer, contributes to cardiovascular health and even metabolism. Kefir is known for its powerful anti-inflammatory effects and fights viral infections. As a side note, kefir has been speculated to reduce or prevent cytokine storm associated with Covid 19.

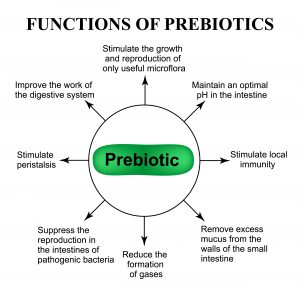
Prebiotic rich foods
A substance called butyrate is a short-chain fatty acid produced by your gut microbes when they break down dietary fiber. Butyrate has numerous health benefits. butyrate is produced when your gut microbes transform the dietary fiber you eat into these beneficial compounds. These compounds help feed the beneficial bacteria in your gut lining; without butyrate your beneficial bacteria wouldn’t survive. Butyrate is made from prebiotic rich foods that your intestine ferments and digests food. Foods high in fiber promote butyrate production such as whole grains, legumes, berries, fresh fruits, and vegetables. Inulin, a prebiotic fiber found in Jerusalem artichokes, chicory root, unripe(green) bananas, and asparagus has been found to positively modulate bacterial diversity during antibiotic therapy
A probiotic called Saccharomyces Boulardii (Trade name Florastor) has been shown to help prevent antibiotic related diarrhea and fight candida infections while on antibiotic therapy. It is a beneficial yeast and not a bacteria, so it isn’t affected by antibiotics. Saccharomyces Boulardii should be taken during antibiotic therapy and for a month after or as your healthcare provider recommends.
Reinoculate
Along with the above recommendations a good probiotic supplement may be necessary to restore gut health. Due to supply chain issues the probiotic I would recommend is no longer available, however here is a link-perhaps you may be able to source a similar product- check with your healthcare provider which probiotic they recommend.
Repair
To repair damage caused by illness and antibiotic therapy Supplementation with L-glutamine, vitamin C and zinc may be necessary. A good quality, balanced multivitamin is also a good idea.
Continue with above recommendations and make this change a permanent lifestyle.
In conclusion
As we enter this time of supply chain disruption and uncertainty the one asset, we and our loved ones have is our health. Without that nothing else matters.